A significant overhaul of the United States’ childhood immunization guidelines has resulted in a reduction of recommended vaccines from 17 to 11 diseases, a move that has ignited both praise from the Trump administration and sharp criticism from leading medical organizations. The updated list, released by the Centers for Disease Control and Prevention (CDC) on Monday, now prioritizes vaccines for a core set of diseases, while others, including those for hepatitis A, hepatitis B, and COVID-19, will be administered based on individual risk assessments and a process of "shared clinical decision-making" between healthcare providers and parents. This paradigm shift in public health policy is being hailed by proponents as a victory for scientific integrity and parental autonomy, while opponents warn of potential public health crises and a dangerous erosion of trust.
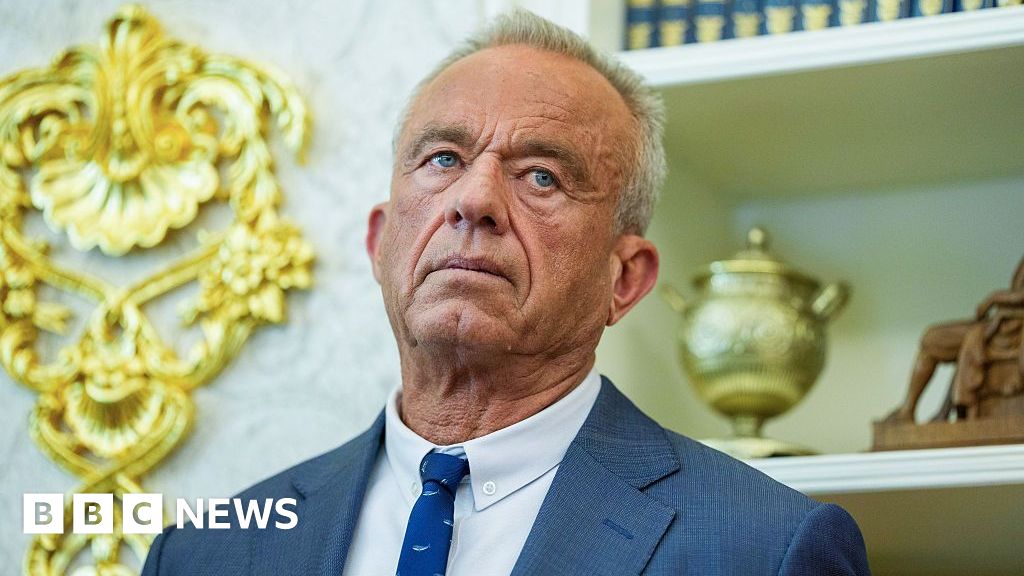
President Donald Trump lauded the revised recommendations, asserting they were "rooted in the gold standard of science." His administration, spearheaded by Health Secretary Robert F. Kennedy Jr., has framed the changes as a crucial step toward modernizing vaccine policy and restoring public confidence. "Many Americans, especially the ‘MAHA Moms,’ have been praying for these COMMON SENSE reforms for many years," Trump declared in an online statement, referencing the "Make America Healthy Again" slogan. Kennedy, who has a well-documented history of skepticism regarding vaccine efficacy and safety, described the overhaul as the product of "an exhaustive review" aimed at protecting children, respecting families, and rebuilding trust in public health. He further elaborated that the changes "align the U.S. childhood vaccine schedule with international consensus while strengthening transparency and informed consent."
The CDC’s updated universal recommendations now include vaccines to protect children against: measles, mumps, rubella, polio, pertussis (whooping cough), tetanus, diphtheria, Haemophilus influenzae type B (Hib), pneumococcal disease, human papillomavirus (HPV), and varicella (chickenpox). These foundational vaccines remain a cornerstone of childhood immunization, reflecting decades of established scientific consensus on their importance in preventing widespread and potentially devastating infectious diseases.
Beyond this core group, a second tier of vaccines has been designated for administration based on specific risk factors. This category includes vaccines for respiratory syncytial virus (RSV), hepatitis A, hepatitis B, dengue, and meningococcal disease (both serogroups ACWY and B, which protect against different forms of meningitis). The inclusion of these vaccines under a risk-based framework signifies a move away from blanket recommendations towards a more individualized approach, acknowledging that the likelihood of exposure and severity of illness can vary significantly among different populations and geographical regions.
A third group of vaccines, comprising those for COVID-19, influenza, and rotavirus, has been explicitly designated as optional, with the decision-making authority resting solely with parents and their healthcare providers. This represents a significant departure from previous policies, particularly concerning the COVID-19 vaccine, which has been a subject of intense debate and public scrutiny. The inclusion of influenza and rotavirus vaccines in this discretionary category also marks a notable shift, as these have been routinely recommended for most infants and children for many years. The CDC has stated that insurance coverage for vaccines currently recommended will continue through the end of 2025, providing a transitional period for families and healthcare systems to adapt to the new guidelines.
These new recommendations stem directly from an executive order signed by President Trump in December, which mandated a comparative analysis of the U.S. immunization schedule against those of "peer developed countries." The U.S. Department of Health and Human Services conducted this comparison, evaluating the U.S. against 20 nations, including the United Kingdom, Canada, Denmark, and Australia. The department concluded that the U.S. was a "global outlier" in terms of both the number of diseases covered by universal vaccine recommendations and the total number of doses administered. Denmark’s immunization schedule, which recommends against vaccination for 10 fewer diseases than the previous U.S. standard, was highlighted as a particular model.
However, this comparative approach and the resulting policy changes have faced fierce opposition from prominent medical bodies. Dr. Andrew D. Racine, president of the American Academy of Pediatrics (AAP), vehemently criticized the comparison and the subsequent recommendations. "The United States is not Denmark, and there is no reason to impose the Danish immunization schedule on America’s families," Dr. Racine stated. "America is a unique country, and Denmark’s population, public health infrastructure, and disease-risk differ greatly from our own." He underscored the vast demographic and infrastructural disparities, noting that Denmark’s population is approximately 6 million, while the U.S. has around 340 million people. Dr. Racine further warned of the potential consequences, predicting that "at a time when parents, pediatricians and the public are looking for clear guidance and accurate information, this ill-considered decision will sow further chaos and confusion and erode confidence in immunizations." He concluded with a stark assessment: "This is no way to make our country healthier."
The AAP’s criticism is not isolated. Republican Senator Bill Cassidy, a medical doctor from Louisiana, also voiced his disapproval, stating, "Changing the pediatric vaccine schedule based on no scientific input on safety risks and little transparency will cause unnecessary fear for patients and doctors, and will make America sicker." This sentiment highlights concerns about the scientific basis and the perceived lack of transparent deliberation behind the policy shift.
The timing of Monday’s announcement is also noteworthy, coming just weeks after a CDC panel revised the recommended timing for the first dose of the hepatitis B vaccine. Previously, a dose was advised within 24 hours of birth. However, revised guidelines issued in December moved this initial dose to two months after birth, contingent on the mother testing negative for hepatitis B. This specific change was also met with widespread condemnation from pediatricians, with the AAP describing it as "a dangerous move that will harm children." The cumulative effect of these recent policy adjustments has amplified concerns among healthcare professionals about the direction of childhood immunization policy.
The broader implications of these changes extend to the intricate landscape of vaccine development, public trust, and the ongoing efforts to combat infectious diseases. While proponents emphasize parental rights and a re-evaluation of vaccine schedules based on international comparisons, critics raise alarm bells about the potential resurgence of preventable diseases and the fragmentation of public health messaging. The debate over these recommendations is likely to continue, shaping public health discourse and policy for the foreseeable future, with significant consequences for the health and well-being of American children. The emphasis on "shared clinical decision-making" represents a significant delegation of responsibility, placing a greater onus on physicians to engage in nuanced conversations with parents, balancing established scientific evidence with individual family concerns and values. This approach, while intended to foster autonomy, also necessitates robust educational resources for both parents and healthcare providers to ensure informed consent and prevent misunderstandings that could lead to suboptimal vaccination rates. The long-term impact on herd immunity and the overall burden of vaccine-preventable diseases will be a critical area for ongoing monitoring and evaluation.







