
Michelle Roberts and Sophie Hutchinson, BBC News

In a medical breakthrough that was once deemed impossible, doctors at Moorfields Eye Hospital in London have successfully restored sight and prevented blindness in patients suffering from hypotony, a rare and severe eye condition. This pioneering treatment, administered at the world’s first dedicated clinic for the disorder, has shown remarkable success, with seven out of eight patients responding positively in a pilot study. Among them is Nicki Guy, a 47-year-old mother, who bravely shares her "life-changing" story exclusively with the BBC, heralding a new era of hope for those facing vision loss.
"It’s given me everything back," Nicki exclaims, her voice filled with emotion. "I can see my child grow up. I’ve gone from counting fingers and everything being really blurry to being able to see." Her vision has improved so dramatically that she can now read most lines on an eye test chart, just one line away from the legal requirement for driving. This is a stark contrast to her previous state of partial sightedness, where she relied on memory to navigate her home and surroundings and needed a magnifying glass for any close-up tasks. "If my vision stays like this for the rest of my life, it would be absolutely brilliant," she reflects. "I may not ever be able to drive again, but I’ll take that!"

Hypotony, the condition that threatened Nicki’s sight, is characterized by dangerously low pressure within the eyeball. This leads to the eye collapsing inwards, a devastating consequence that can arise from insufficient production of the eye’s natural fluid, trauma, inflammation, or as a side effect of eye surgery or certain medications. Before this new therapy, treatment options were limited and often ineffective. Doctors had previously resorted to using steroids and silicone oil to try and plump up the eye. However, these methods carried risks of toxicity with prolonged use and offered minimal visual recovery. Moreover, even when the light-sensitive cells at the back of the eye remained functional, the silicone oil itself obstructed vision, resulting in persistent blurriness.
The team at Moorfields, driven by a desire to find a more effective solution, turned to a readily available, low-cost, transparent, water-based gel called hydroxypropyl methylcellulose (HPMC). This substance is already utilized in some eye surgeries. The innovative approach developed by the Moorfields team involved injecting this gel into the main cavity of the eye as a novel therapeutic strategy, moving beyond its traditional surgical application. This clear gel, unlike the viscous silicone oil, allows light to pass through unimpeded, enabling clearer vision if the underlying retinal cells are viable.

Nicki’s journey with vision loss began in 2017, shortly after the birth of her son. Her right eye was the first to show signs of decline, losing its normal shape and "sort of collapsing" or "crumpling like a paper bag" due to hypotony. Despite receiving multiple injections of silicone oil, the treatment offered little improvement. A few years later, her left eye began to deteriorate in a similar fashion. "After I lost vision in my left eye, I thought, ‘there has to be something else we can try’," she recalls, her determination evident. "Sheer determination. I was just like ‘I’m not giving up’."
Her eye doctor, Mr. Harry Petrushkin, acknowledged the significant risks involved in such an experimental procedure. "The idea that we might be causing harm to somebody who has only really one eye with a treatment that may or may not work was nerve-wracking," he admitted. "We came up with this as a solution and amazingly it worked. Really, we could not have dreamt of her having the outcome that she has had. Somebody, who by all rights should have lost her vision in both eyes… is now living normally. That’s completely remarkable. We couldn’t have hoped for better."
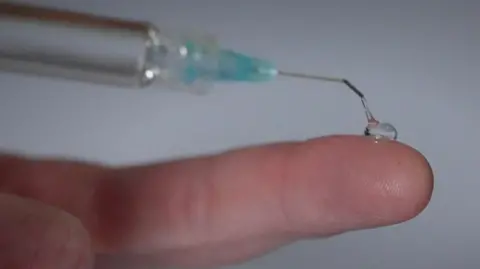
The revolutionary treatment involves injecting the HPMC gel into the eye every three to four weeks for a period of approximately 10 months. This sustained delivery of the gel helps to maintain intraocular pressure, allowing the eye to regain its normal shape and function. The clarity of the gel is crucial, as it doesn’t impede the passage of light to the retina, the light-sensing tissue at the back of the eye. When light signals are captured by healthy retinal cells, they are transmitted to the brain via the optic nerve, restoring vision.
Mr. Petrushkin believes this treatment holds the potential to benefit hundreds, if not thousands, of individuals in the UK annually who are affected by hypotony, provided they still possess viable retinal cells. "We knew with Nicki there was vision to gain and she would get better if we could make her eye round and hard again."

To date, the team has treated 35 patients with this innovative therapy, supported by funding from the Moorfields Eye Charity. The initial findings from the first eight patients have been published in the prestigious British Journal of Ophthalmology, showcasing the promising outcomes. While the results are highly encouraging, Mr. Petrushkin emphasizes that it is still early days. "It’s been a fantastic story. The results are really promising but it’s early days," he stated. The researchers are optimistic that with continued study and experience, they will refine their understanding of which patients are most likely to benefit from this groundbreaking treatment, further expanding its reach and impact. The success with Nicki Guy serves as a powerful testament to the relentless pursuit of medical innovation and offers a beacon of hope for those battling sight-threatening conditions.








