Larissa Hope, a former actress, firmly believes psilocybin was instrumental in navigating a severe mental health crisis during her adolescence. At just 17, while starring in the acclaimed TV drama Skins, the sudden glare of fame inadvertently unearthed a deeply buried trauma. Traditional antidepressants proved ineffective in alleviating her distress. It was a single, carefully administered dose of psilocybin, taken under rigorous clinical supervision, that marked a profound turning point in her journey. She recalls the experience vividly, describing an overwhelming emotional release. "When I experienced it, I burst out crying," she recounts. "It was the first time in my life I had ever felt a sense of belonging and safety in my body. I kept saying, ‘I’m home, I’m home’." Nearly two decades later, Larissa maintains that this singular experience, coupled with ongoing therapy, empowered her to confront and overcome persistent suicidal ideation, ultimately saving her life.

However, not everyone shares Larissa’s positive experience. Jules Evans, a university researcher, offers a starkly different perspective, rooted in his own encounter with psychedelics. At 18, he consumed LSD recreationally, an experience that spiraled into what he describes as a "deluded" state. "I believed that everyone was talking about me, criticising me, judging me. I thought, I’ve permanently damaged myself; I’ve permanently lost my mind," he says. "It was the most terrifying experience of my life." The repercussions were long-lasting; he battled social anxiety, panic attacks, and was eventually diagnosed with post-traumatic stress disorder (PTSD) years after his trip. Today, Evans directs the Challenging Psychedelic Experiences Project, an initiative dedicated to supporting individuals who encounter difficulties following psychedelic use. His work highlights the critical need to understand and address the potential adverse effects, ensuring that any move towards medicalisation is underpinned by comprehensive safety protocols.
These two profoundly contrasting narratives underscore the core dilemma confronting doctors, regulators, and policymakers across the UK. The central question is whether the medical establishment should sanction treatments involving magic mushrooms and other potentially therapeutic psychedelic drugs, moving them from the realm of illicit substances to legitimate medical interventions.

The resurgence of interest in psychedelic medicine is driven by a growing body of new studies. These investigations suggest that psychedelic drugs hold promise in treating a wide array of mental health conditions, including severe depression, obsessive-compulsive disorder (OCD), PTSD, complex trauma, and various addictions such such as alcohol and gambling. Currently, the medical use of psychedelic substances remains illegal in the UK, save for their deployment within authorized research or clinical trials. Since 2022, over 20 such trials have been underway, rigorously testing different psychedelic compounds for conditions like depression, PTSD, and addiction. While many of these studies have yielded encouraging results, indicating potential benefits, others have presented mixed or inconclusive data. Crucially, only a handful have definitively shown no benefit on their primary outcome measures, maintaining overall scientific optimism.
A pivotal moment is anticipated later this year with the release of results from one of the largest clinical trials involving psilocybin, conducted by the UK biotech firm Compass Pathways. The UK’s medicines regulator, the Medicines and Healthcare products Regulatory Agency (MHRA), is keenly awaiting this data as it deliberates whether to ease existing stringent restrictions and permit the use of psychedelic medicine outside of research and trials. Prof Oliver Howes, chair of the Royal College of Psychiatrists’ Psychopharmacology Committee, expresses cautious optimism regarding psychedelics as a potential new frontier in psychiatric treatment, particularly for NHS patients. "One of the key messages is that this is something we desperately need – more treatments and better treatments for mental health disorders," he states. He highlights the "really interesting" promise shown in smaller-scale studies and the potential for these treatments to act more rapidly than conventional therapies. However, he also stresses the paramount importance of robust evidence from large-scale trials, urging against "overhyping the potential benefits." This sentiment is echoed in a report published by the Royal College of Psychiatrists in September 2025, which issued warnings about the potential dangers of psychedelics and reiterated that recreational use remains illegal and potentially harmful.
The use of psychoactive substances for various purposes dates back to ancient civilisations, with magic mushrooms, opium, and cannabis featuring prominently in both recreational and ritualistic contexts. In the mid-20th century, a wave of scientific research into psychedelics like LSD gained momentum, but this was swiftly overshadowed by their association with the counterculture movement of the 1960s and 70s. Figures like Harvard psychologist Timothy Leary famously exhorted young people to "turn on, tune in, drop out," advocating for a radical shift in consciousness and societal engagement. This cultural phenomenon ultimately led to these drugs being linked with social unrest and perceived moral decline, culminating in their widespread ban in the late 1960s and early 1970s. The prohibition not only curtailed recreational use but also imposed severe restrictions on scientific research.
However, a new era began in the 2010s with groundbreaking scientific developments led by Prof David Nutt and his team at Imperial College London. Their work initiated a process that may well reverse decades of prohibition in the medical sphere. Subsequent clinical trials involving depressed patients indicated that psilocybin could be at least as effective as conventional antidepressants, and crucially, with potentially fewer side effects. Prof Nutt also highlighted another significant advantage: its rapid onset of action. "We thought rather than wait for eight weeks for antidepressants to switch off the part of the brain associated with depression, maybe psilocybin could switch it off in the space of a few minutes," he explained, suggesting a paradigm shift in treatment approach. While scientifically promising, this view is not yet universally accepted without further large-scale evidence. Prof Nutt, a respected scientist, has not been without controversy; his dismissal in 2009 as chair of the government’s drugs advisory body followed public comments comparing the harm of horse-riding to ecstasy, which were deemed incompatible with his advisory role. Nevertheless, his pioneering studies have undeniably spurred a global resurgence of investigations into the therapeutic potential of various psychedelic drugs.
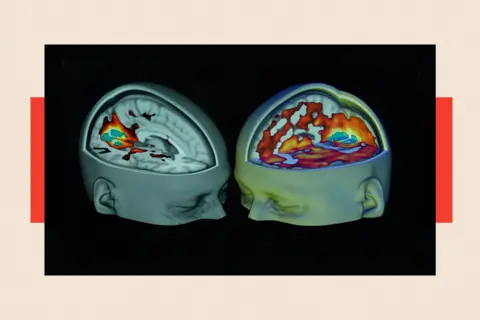
The ultimate question remains: should these treatments be made available on the NHS? At University College London, neuroscientist Dr Ravi Das is exploring how habits solidify into addictions and how psychedelics might offer a solution. His ongoing study recruits heavy drinkers to investigate whether dimethyltryptamine (DMT), a short-acting psychedelic, can target the brain’s memory and learning systems. This research builds on existing evidence suggesting psilocybin can disrupt the habitual behaviors associated with addiction. "Every time someone drinks, a bit like Pavlov’s dog, you’re learning to associate things in the environment with the rewarding effect of alcohol," Dr Das explains. "We’ve been focusing on whether certain drugs, such as psychedelics, can break down those associations." This is an early-stage study, but if successful, the aspiration is to offer it as an NHS treatment, subject to regulatory approval. Dr Das argues for equitable access: "If psychedelic therapies prove to be both safe and more effective than current treatments, I would hope to see them made accessible via the NHS – rather than to just the privileged few who can afford them privately."
The legal status of various psychedelics differs significantly. Ketamine, for instance, operates under a different legal category and is already used as part of medical treatment in the UK for certain conditions. In contrast, DMT, LSD, psilocybin, and MDMA are currently classified as having no legitimate medical use, confining their application strictly to highly regulated research with difficult-to-obtain medical licenses. Dr Das remains hopeful that accumulating positive scientific evidence will prompt the government to reconsider and revise the scheduling of these drugs.

However, an analysis published in the British Medical Journal in November 2024 by PhD student Cédric Lemarchand and his colleagues urged caution, highlighting the inherent difficulty in precisely determining the effects of psychedelic drugs. "Because hallucinogens are often combined with a psychotherapy component, it is difficult to separate the effects of the drug from the therapeutic context, complicating comprehensive evaluations and product labelling," the analysis noted. It also raised concerns that short-term trials might not adequately detect "the potential for harm and serious adverse events from long-term use of hallucinogens… The potential for abuse or misuse must also be considered."
While research consistently points towards the therapeutic benefits of psychedelic medicines, medical professionals like Prof Howes maintain a cautious stance. He argues that, with the exception of ketamine which has undergone regulatory assessment, psychedelic treatments should not become routine medical practice in the UK outside of controlled research settings until larger, more rigorous trials provide robust evidence of their safety and effectiveness. "In a clinical trial setting, it’s very carefully evaluated. If people take these on their own or in a backstreet clinic, then there is no guarantee of that, and the safety issues start becoming a major issue," he warns. These warnings are supported by data from the Challenging Psychedelic Experiences Project, which indicates that 52% of regular psychedelic users have reported intensely challenging trips, with 39% considering it "one of the five most difficult experiences of their life." Furthermore, 6.7% reported contemplating self-harm or harming others following a challenging experience, and 8.9% experienced impairment lasting more than a day. Jules Evans notes that some individuals required medical or psychiatric assistance and continued to suffer for weeks, months, or even years after their adverse experiences. "Ideally, I would love doctors and regulators to know more about these adverse effects, and how people can recover from them, before they say any of these therapies are safe," he contends.

Despite these necessary cautions, proponents like Prof Nutt, Prof Howes, and Dr Das lament that progress in bringing these therapies to the clinic is painfully slow, primarily due to the arduous process of obtaining permission for medically supervised clinical trials. "There are so many people suffering unnecessarily," Prof Nutt told BBC News. "And some of them are dying, because of the unreasonable barriers to research and treatment that we face in this country. It is, in my view, a moral failing." He asserts that once these medicines are proven safe and effective, it is "vital they are made available through the NHS to all who need them, not limited to the private sector, as happened with medical cannabis." Prof Howes, while advocating caution, shares this view, stating, "There are big barriers to doing this research, so we do ask for the government to review the regulations of these substances, for research, because it does lead to long delays, and, we desperately do need new treatments."
The BMJ analysis by Lemarchand further advocates for greater scrutiny of trials, insisting that "to guarantee that hallucinogens are rigorously vetted before endorsing them as safe and effective treatments, medical journals must appraise the evidence more critically, fully account for limitations, avoid spin and unsubstantiated claims, and correct the record when needed." The Advisory Council on the Misuse of Drugs remains resolute, stating that Schedule 1 substances, which include most psychedelics, contain "no medicinal value" and thus warrant the tightest controls, a stance echoed by ministers who link the Home Office licensing regime directly to public protection.

The government has acknowledged the need for change, backing plans to ease licensing requirements for certain clinical trials approved by the MHRA and Health Research Authority. Work is underway to implement exemptions for specific universities and NHS sites, with a cross-government working group coordinating a cautious rollout pending the results of pilot projects. However, doctors like Prof Howes feel that changes are progressing at a frustratingly slow pace. "There’s still a lot of red tape holding things up," he notes.
Supporters of psychedelic medicines hold out hope that the upcoming phase three trials by Compass Pathways will pave the way for further relaxations, at least concerning research. Larissa Hope, whose life was profoundly changed by psilocybin, underscores the critical importance of these trials. She credits her experience with helping her gain invaluable insight into her suicidal ideation and trauma. "I had a solid plan to end my life. Then suddenly, death wasn’t the only way," she reflects. "Under psilocybin, my nervous system began, for the first time, to recognise what peace felt like."








